Chronic thromboembolic pulmonary hypertension (CTEPH) is a fatal but curable disease afflicting the pulmonary arteries. Diagnoses include a mean pulmonary arterial pressure (mPAP) greater than 20 mmHg and unresolved lesions in the pulmonary arteries. CTEPH is widely underdiagnosed since its symptoms (dyspnea, exercise intolerance, malaise) are common in many other diseases, and it is detected only through CT imaging and right heart characterization. One treatment for these patients is balloon pulmonary angioplasty (BPA), where stents are inserted into blood vessels and inflated to increase blood flow past embolisms. Currently, there is no systematic way to determine which lesions to treat to maximize outcomes: increasing perfusion and decreasing pressure. To remedy this, we devise a personalized one-dimensional (1D) fluid dynamics model predicting blood pressure and flow in the pulmonary arteries. Using this model, we will compare outcomes in control and patient networks. To simulate treatment, we will remove different combinations of lesions in personalized networks generated from CT images to optimize prognosis.
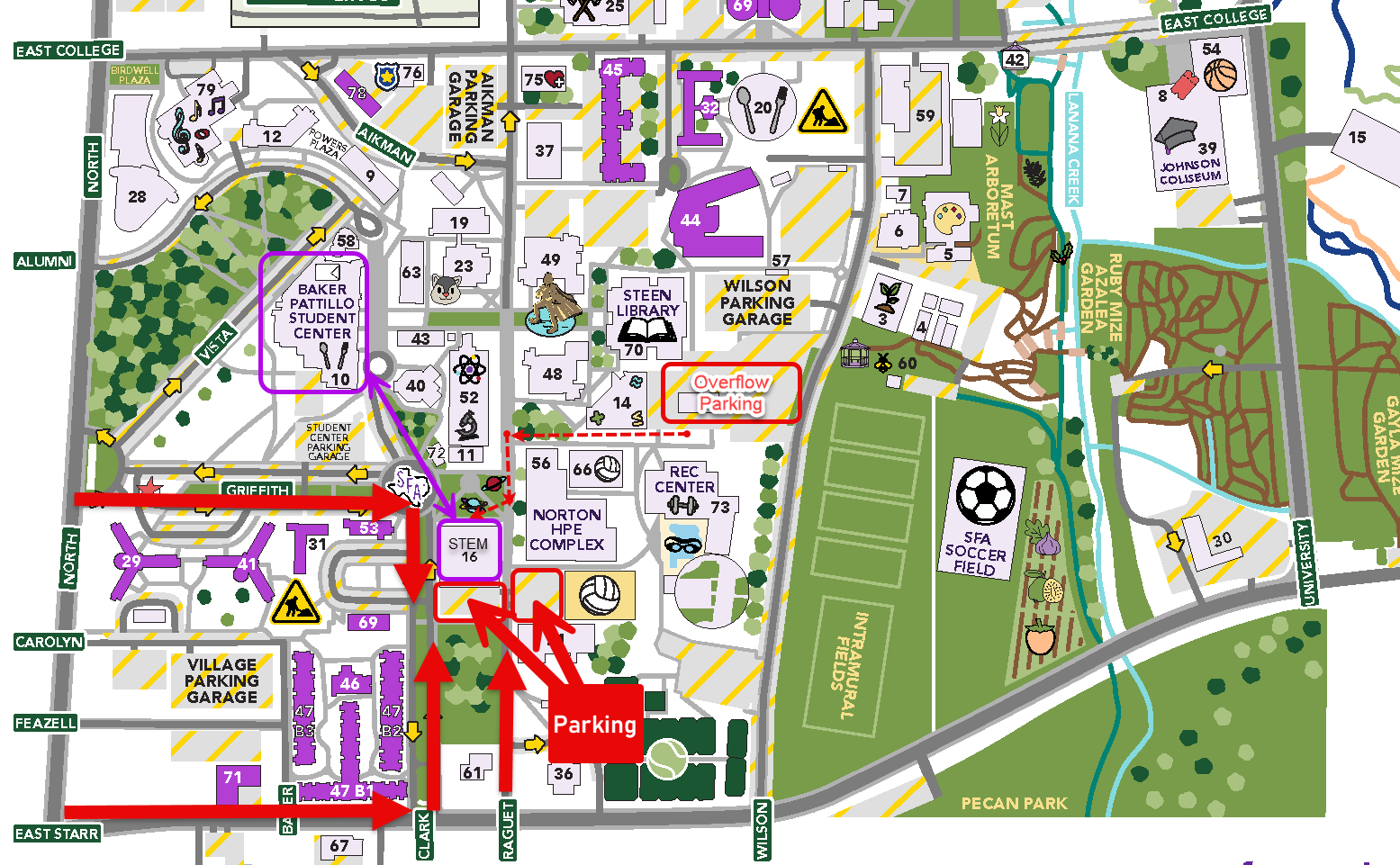
Using 3D Slicer, we generate 3D volumetric surfaces (segmentations), and from these, using the Vascular Modeling Toolkit (VMTK), we extract centerlines along each vessel and connect them in a labeled tree. Nodes along the centerline each have an associated radius and coordinates in 3D space, and the connection of nodes along a vessel gives us vessel length. Junctions form when nodes intersect, and we represent a network of vessels through a connectivity matrix. To find a representative radius, we average the radii of relevant nodes, identified using our change point algorithm. This algorithm determines vessel radii and its uncertainty and corrects junctions between vessels to be more physiologically accurate. We pruned networks until they had the same number of arteries to standardize networks. Then, we attach asymmetric binary trees at the end of each terminal vessel to extend our network past resolution limits in CT scans. We solve a 1D fluid dynamics model in this network, predicting blood pressure and flow in each vessel.
Preliminary results predicting mean pulmonary arterial pressure and flow in five segmentations from a healthy control’s pulmonary arteries show that the size of the tree matters, and, using ANOVA analysis, we found that vessel radii and length differ significantly between segmentations; however, sampling from the radius estimates for each vessel provides reliable predictions of pressure and flow. Segmenting CTEPH patients reveals multiple lesion types per patient, including ring lesions, total occlusions, and tortuous vessels. Future work includes generating CTEPH networks and conducting fluid dynamics simulations in CTEPH geometries. These in-silico treatments and simulations mitigate the need for invasive and expensive scanning and provide insight into optimal treatment plans for physicians.